 Sometimes we just need a pause. Sometimes we need momentum. Sometimes we need healing. I feel like I received all that and more during my recent continuing education experience. I’ll spare you the rabbit trail of how I stumbled across it, but I am so grateful that I did and that the timing to be able to attend worked out so well. So, what did I do? I attended a postpartum sealing workshop in California! (May also be referred to as “bone closing”). I wanted this for so many reasons. The shock and aftermath of my own postpartum experience three years ago forever changed me. The life it almost took has been reborn with passion and purpose to reach out to others. You are not alone! You may feel broken or altered, but as long as you keep searching, moving one foot in front of the other by any measurable, albeit minute effort, there is hope. There is excitement, so much excitement, but there is also still some learning and fleshing out to do before I feel truly confidant to go forth. At this time I plan to gather the things that I need and try out this method/process on a few people who have passed the traditional immediate postpartum period of 6 weeks. Why? I genuinely want to be authentic in this healing. I don’t want to just run through the steps and seem inorganic in any way. This healing is a process and there are multiple steps, that I will share in more detail after my “practice period.” A super-condensed look at it starts with a steam, then a hot bath followed by wrapping, massage, and abdominal wrapping. It almost does the process injustice to list it with such brevity, but I can assure you the process is warmth and it gives love and healing. It is not only time-consuming, but also incredibly taxing on the provider; which saddens me because my original goal was to offer this option to all new mothers, not just women who delivered with me. This reinforced a lesson I’ve learned in that I have to pace and preserve myself so that I am at my best in order to offer my best. I may still be able to offer 1-2 spaces each month for this as a stand-alone service during the months I am not already booked with midwifery clients, but at this point I can’t say for sure. Ultimately this process is done between 7-14 days following childbirth, but for many women it is healing no matter how much time has passed since her last child was born.
0 Comments
 During the pregnancy and after baby’s arrival, I remind my clients that I am not a pediatrician. The law does allow for midwives to care for babies for up to six weeks, but I encourage the parents to find a pediatrician and discuss how soon they should be seen. Most often, I am still the first one to see the baby by this 24-48 hour home visit window. Lots of things happen during this visit for the baby. It is important to do a nursing check and help if there have been any difficulties with latch. If nursing is going well, then not as much time is needed there. We check baby’s vital signs including his/her heart rate, respirations, temperature, and review the chart that the parents have been using to track how baby has been doing in the time the midwife was gone. We review how many wet and dirty diapers that the baby has had, how much indirect sunlight the baby is getting (this helps to break down bilirubin levels and can help to prevent jaundice), and how baby is sleeping. This is the ideal window to collect that first sample for the newborn screening and to perform the CCHD(Critical Congenital Heart Defect) screening. The baby is of course weighed, and we discuss how much weight loss is okay versus too much, as it is NORMAL for the baby to have dropped weight during this time. Because I do not have the equipment to perform the hearing screen, I remind the parents they will need to have this done either by their pediatrician or through another provider I refer. Following baby’s checkup, he/she may be brought into the herbal bath with mom. If the baby will be in the bath, we delay applying the cord care powder to the umbilical cord until after the bath. I also use this time, if we didn’t already review it during the first herbal bath following the birth, to show the parents how easy bathing a newborn while in the tub with them can be. You’d be amazed at how overwhelming it can seem to bathe a new baby! I want everyone to feel comfortable and confident in this time! The baby is dried, diapered after applying olive oil to his/her bottom (GREAT tip for helping that tar-like meconium to slide right off!), the cord is examined and treated, and the baby is dressed and wrapped or ready for skin-to-skin with mom or dad. You were able to deliver your baby at home, everything was normal and stable, and the midwife left you and baby snuggled up, resting in bed. I like to remind my clients to call me after their recovery sleep and after they’ve had some time to settle in a bit to let me know how nursing is going and to ask any questions that may have popped up in this time. Letting them call me helps to avoid me waking them with a phone call and instead allows the new parents time to adjust and do things on their schedule. If we didn’t set a time following the birth for the postpartum home visit, we typically schedule it at this time. The timing of the first home visit to check on mom and baby is anywhere from 24-48 hours following the time of birth. Of course, if there are any concerns, the midwife returns as appropriate. While the particular timing is mostly due to the ideal time to collect a blood sample from the baby for the purpose of the first newborn screening (the test used to check for a myriad of metabolic disorders), it is also a great time to check in on mom to be sure she is remaining stable. Keep in mind that mom and dad (or perhaps another family member who was appointed for the task) have been keeping note of some vitals for the mom and baby in the time between immediate postpartum period and this first home visit. I work to make sure parents feel equipped for this and are not overwhelmed with this responsibility. When I arrive, after washing my hands and greeting my clients and the new baby, I set out to boil another pot of herbs so that mom can take another herbal sitz bath. I didn’t used to do this routinely at this postpartum visit, yet I found all too often that when I asked if they had done any more herb baths since the birth, the answer was typically that they had not. My initial focus is on mom, addressing any questions or concerns she has. I check her vital signs, feel her fundus (the top of her uterus), we discuss how her bleeding has been and any pain/discomfort she may be experiencing (from breasts/nipples to a sore bottom). We discuss her nutrition and her supplements since the birth. It is important to remember that a nursing mother needs more calories when breastfeeding than she did when she was pregnant! (A pregnant mom typically needs about 300 calories over what her normal was prior to pregnancy. A breastfeeding mom typically needs about 500 calories over her pre-pregnancy allowance.) Many times it is through the discussion about supplements that a mom is reminded she should be continuing to take them. For many, it is an “out of sight, out of mind” issue. We have been encouraging moms to rest and take it easy, which typically means they are remaining in the nest of their room. This has pros and cons for sure! This protected isolation from the world can also deter some of the self-care they were so careful to instill during their pregnancy. While discussing and addressing the various topics above, I am getting a sense of how rested mom is and a glimpse of her outlook and emotional state. I also ask directly how she is doing emotionally and whether or not she’s been able to fall asleep during her rest periods or if she’s just putting her feet up and taking it easy. Following the mom’s assessment, we help her into her herbal sitz bath, bring her something to drink, and give her some time to herself while dad stays with the baby during his/her assessment. I have seen mothers light up with this opportunity to have some uninterrupted time in the herb bath. This is addressing her physically as well as emotionally. Sometimes, I have brought the baby to them at the conclusion of the baby’s exam and procedures, and sometimes they prefer that I don’t. The choice is yours. Those that choose to have the baby brought into the herb bath may choose to nurse the baby while in the tub, or simply hold the baby and help them to float, enjoying the warm bath. Once mom and baby are ready to be helped out of the tub, the baby goes to dad and I help mom to the bed. During this time I demonstrate an abdominal massage and binding to help the mother feel supported and to encourage healing. The partner gets to see how they can be a part of this healing process and look forward to being in charge of providing the massage for the next couple of days. To my former clients who are reading this and thinking things sound a bit different, you are right. Some of you are currently with me for another round and you WILL experience this. I am putting into practice new things as I grow and learn. I am blessed to have the opportunities to share this and find it providential that these changes occur and benefit the postpartum period. If you are “done done” having children, stay tuned…there is more. The postpartum home visit is more than just a checkup. You are addressed physically as well as emotionally. I want to leave you feeling as though you matter, you are important, you are more than your birth, you are more than “just a mom”, you are (insert your name here)! Similar to my departure following birth, I like to leave mom and baby resting comfortably together in bed, well attended and nourished. 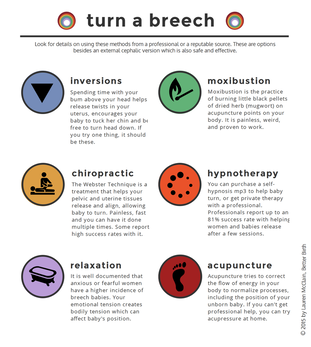 Hi! You’re probably anxious and have a million things running through your mind if you’ve come to this blog post. I will start off by encouraging you to relax. Let’s take this one step at a time. Your baby is breech, or isn’t head down. Is this a problem or something to be concerned about? How far along are you? A baby who is breech at their 20 week anatomy scan (ultrasound) isn’t a cause for concern. He/she has plenty of time to turn. A bit further along? Let’s break it down. As a midwife, I’ve seen this before. As a mother, I’ve experienced this before with my last pregnancy. What I’ve come to find is that there is a “sweet spot” with regard for optimal time to turn baby that usually results in them staying head down for birth. Is that ALWAYS the case? Has every breech baby I’ve encountered turned head down and resulted in a vaginal birth? No. But overall, the following methods are worth a try to see if they may help you. So, what can you do?
When would you need to consider starting these? That depends on how far along you are and how long baby has been in a breech position. If the first time you’re hearing about this is 33-34 weeks, you may consider starting with the appropriate homeopathic remedy, which will depend on whether there is an issue of over- or under-abundance in amniotic fluid levels or not. Different remedies are suggested based on the whole picture, not just baby’s position. Do your research or seek out a homeopathic healthcare provider who can help. Beginning at 34 weeks: Optimal Fetal Positioning TechniquesYou may have heard of Spinning Babies? Check out their website fo more specific exercises and to expand on this information: www.spinningbabies.com This is also a great time to begin chiropractic adjustments with a provider who is pregnancy certified, if you haven’t already. Perhaps baby is “stuck” in a certain position due to tight ligaments. 35 weeks gestationThis is what I found to be the “sweet spot” with regard for timing. The previous times we tried to encourage my little guy to turn, he just moved right back into the position he was in. Doing the ironing board technique coupled with the cold pack on his head (top of my belly) and heating pad on my lower abdomen (above my pubic area) made him turn at that time and because he wasn’t too little, he stayed that way! If the above tips haven’t helped baby to turn just yet, you may want to consider acupuncture. It’s actually very relaxing and can have great results. Finally, if around 37 weeks baby has not yet turned, your healthcare provider may have set up a consultation to see if you are a good candidate for an external cephalic version or ECV. Basically, that’s a procedure where your baby is turned or encouraged to turn by the hands of the provider, usually while monitoring baby via ultrasound. What if baby has been consistently Breech at 28, 30 & 32 week visits? (Or 2 out of 3 of those visits)You may consider starting the homeopathy, chiropractor and acupuncture earlier, giving yourself more time. Remember, most babies turn before delivery. I’d encourage you to wait rather than scheduling a surgical birth at 37 weeks for a baby who has not turned. If this is your first baby, the average is to go 10 days past your due date! That means baby would have a month to turn! Meanwhile you can be doing the above tips and techniques to encourage him or her to do so.  You’ve reached your estimated date of delivery. Now what? Last fall, one of my clients reached out about waiting. This was her third pregnancy, but she had already delivered by this point during her previous pregnancies. She stated she didn’t understand why this time was different. She understood there wasn’t a rush; however, there was a fear about the possibility of needing medical intervention to get the ball rolling. Pregnancy is a process. While not everyone’s experiences are the same, I think most women would agree they learned something about themselves during their own journeys. Some women are pleasantly surprised to find they go into labor unexpectedly days or weeks before the BIG EDD! Others of us know, from day one, that is not likely to happen for us, due to our own previous experiences or a family history of holding onto those babies for days or weeks longer! From my own experience, I understand completely! During my third pregnancy, I was working a corporate job and couldn’t wait for the day after my due date to arrive so that when I was asked again “When are you due?” I could smile and respond “Yesterday,” just to see the looks on people’s faces. Priceless. Interestingly, most people aren’t used to that response, especially in work environments, for numerous reason (scheduled deliveries, people taking leave at or prior to that time, etc…). Perhaps you are one of the frustrated momma’s who went into labor weeks early with your first, and now you are shocked and beside yourself for going past that special date. I believe this is the most frustrating position, because you could literally be pregnant a month longer than your previous experience! All I can say is, I’m so sorry! I do speak with those clients up front and throughout their pregnancy about this possibility, to help to keep the angst down as much as possible. Let’s say you find yourself here, 40 weeks on the dot, without any reportable signs or symptoms of impending labor…now what?!?! I like to take a 3 step approach, in order to address your mental outlook, your emotions and your physical needs.First, most people like to have a plan in place. It helps them feel prepared and a little more in control. I know there is very little that can be controlled in life, let alone in pregnancy, but for myself I find that it helps to do what I can to help as much as I can. So, I review what things look like now that we’ve reached 40 weeks. For some, it may mean prenatal visits two times a week instead of weekly, though for others that doesn’t happen until 41 weeks. I recommend clients have a BPP (biophysical profile) done at 41 weeks. (Read about this in an upcoming post). We discuss a general overview of what to expect at those appointments, and any steps that can be taken between appointments to help ripen the cervix (supplements/activities). I also explain what happens if in fact we make it to 42 weeks, and the process of a medical induction. Personally, I feel exploring the upcoming two weeks at that time is more assuring because then my clients know what to expect. I also feel that discussing it all minimizes the likelihood of needing to go that far, versus not talking about it and everyone being frustrated, upset or confused if indeed we end up there. I educate in order to empower. Second, I address the emotional component. It’s one thing to know in your head logically what is happening and what is to come, but that doesn’t address your feelings about it. This is a bit more difficult to quantify, because this is when my relationship with my clients comes more into play. One client may have fears about the “what ifs,” another may be anxious, while yet another may be actually angry about the wait. There are LOTS of emotions that come out in pregnancy and typically if you don’t see it early, you see it towards the later part. I was taught and like to use the analogy about a piece of fruit. Fruit is best when it is ripe, and sometimes it feels as though that will come any day, and sometimes you keep checking back only to have to wait a little longer. Then, you have this window of time where you can enjoy the fruit at its peak, when it is at its best! If you happen to go past this time, the fruit turns rotten. While for fruit purposes you’d throw it out because it wouldn’t be so pleasant to enjoy it, when you turn the analogy back to an expectant mom who has crossed this ideal window emotionally in her pregnancy, this is the time she realizes she is ready and she’s willing to do anything (Endure Labor!!) to get this baby out! Why does this help? Because sometimes emotionally we are holding on a bit, perhaps fearful of labor, of pain or of the unknown. Separately, I encourage my clients and build them up, ideally so that they leave with hope and uplifted spirit. I also encourage a date night, no matter when the last date night had been, so that they can get some uninterrupted time with their partner. This connection shouldn’t be taken for granted. Oftentimes, after a date day, labor is just around the corner. This is good for SO many reasons, but mostly the communication that takes place helps to unlock some things that were meant to be talked out before baby comes. Lastly, we address your physical needs. Again, this is tailored to each client, but may include suggestions of getting some “you time,” a night out with friends or time alone to take a long bath or read. Overall, my recommendation is to have something planned each day. I’m not talking something big and crazy, I’m just talking one appointment to set for yourself – it could literally be a reminder on your phone to have lunch with a friend, not necessarily a massage appointment, but that works too!!! With my first pregnancy, my mom scheduled a hair appointment on my due date, feeling pretty certain I would need the distraction. While I was a little bummed to still not have my baby in my arms, the appointment gave me something to look forward too and I felt really good about myself afterwards! The idea here is to have something to look forward to each day, even if it’s knocking another item off your “to-do” list that you wouldn’t mind cancelling, if in fact you were to go into labor. Outdoor activities or anything out of the house is ideal since it may be a little while before you are venturing out after baby arrives. I am VERY careful to stress balance at this stage, which is why I recommend just the one thing or appointment a day. Balancing activity and rest towards the end of your pregnancy is key in setting yourself up for being as well-nourished and rested as possible before going into labor. Remember, it could happen any day and while we are trying to shift your focus temporarily from that, it is a reality that you need to be prepared for. On average, first time moms go into labor 10 days following their expected date of delivery, or 41.3 weeks! Remind yourself of that and take the above suggestions and adapt them to make them work best for you.  What is a Monitrice?A monitrice is similar to a doula with some added benefits. As a licensed midwife I am able to offer the extra services of monitoring your baby’s heart rate, taking your vital signs and performing cervical exams (if requested) to help ascertain the appropriate time to head to the hospital so that you can enjoy the comfort of your home in that early stage of labor. Support for Hospital BirthsGenerally this option includes 1-2 prenatal visits, labor support for the birth itself and a follow up postpartum visit. I will:
Recently, I had an opportunity to attend an acupressure workshop for birth workers. I was on the fence originally, as I had missed the early registration deadline and had already been away from my family attending another training for five days not so long before this, but something kept nudging me to go. When I read all the information, saw the fee was 100% refundable if the workshop was missed for a birth (this is HUGE for midwives), it was local (equally as important when clients are in range to deliver), and my husband encouraged me to go knowing it would help me and my clients (this helped alleviate “mom guilt”), I was IN!
The workshop itself was informative, and I loved that we were hands-on practicing right then and there. My only issue is that I wasn’t experiencing any of the ailments the day of the workshop that we were learning, except for a neck issue from my car accident back in June. That being said, I have to be honest, I’m a bit of a skeptic by nature; so, without experiencing first-hand drastic relief or improvement, I wasn’t sure what I’d actually walk away with. I was appreciative for the presentation and for the documents provided so that we could practice and use as indicated for ourselves and our clients. It was probably about a week following the workshop that my next client went into labor. This would be her second child, and first out-of-hospital birth. She was about 6cm dilated when I arrived but I wasn’t loving how the baby’s head was applied against the cervix. That’s when I decided to give my new tool a try. Fortunately, in preparation for the birth, I had scanned in the handouts to be accessed from my phone. I scrolled through to find the points that were most indicated for a posterior or asynclitic baby (fancy term that basically means the head is cocked funny or not well tucked-chin to chest). We had already gotten mom’s vitals and listened to baby, and since everyone was doing really well, we proceeded with a circuit of 3 positions for mom while dad supported, and we held some acupressure points. She started out on her hands and knees, which on its own is a fantastic position for helping baby’s position, for 10 minutes, then got onto her bed and did four contractions lying on her left side and four contractions lying on her right side (the opposite leg is bent and supported with a pillow folded just in front of mom’s belly/baby). Afterwards she got up to use the restroom while I charted a couple things and told her she can do anything that seemed comfortable and encouraged her to listen to her body. Literally within minutes her contraction pattern intensified. (Note: a less than ideal presentation can cause ineffective contractions or longer labors.) She decided to get into a warm bath for comfort and just changed positions as she desired, mostly kneeling. At this point, we were helping with her comfort, hydration, and listening to baby’s heart rate as she navigated transition. I could tell something had changed and asked what she was feeling with the contractions now. She no longer felt the pain above her pubic bone, she just said it was different and had more pressure. Deciding to empty her bladder one more time, she was helped out of the tub and onto the toilet. It was in this position that she realized how low baby was, that this was happening now, and that she had the sensation to bear down with the next contraction. She declined the offer to be helped back into the bathtub, so we readied ourselves and supplies to do the delivery where she was. With her first push, the tight and bulging bag of water was visible, and minutes later she was holding her daughter in her arms with the most incredible look of amazement and disbelief on her face. In total, it had been about two hours from the start of the acupressure points and positioning circuit to the time she had birthed her daughter! While I obviously couldn’t promise the same timing and speed for everyone, to me it is evidence that it worked! Most notable to me was the obvious shift that took place in the contractions after our attempt to use the acupressure and positioning to help move baby into a more optimal position for labor and birth. I realize it won’t always be a necessary tool for each birth, but I am thrilled to add it to my toolkit  Recently I was called to step in as a labor support person for a client when her Doula had to attend a mandatory engagement. While not super common, occasionally things come up and necessitate such an arrangement, and I am happy to have a support network I can call on, just as I am proud to support others within this community. The Doula kept me informed of her assessments as the time was drawing near. Upon arrival, I asked to see the contraction app in order to get a picture of recent activity. Contractions were irregular, anywhere from 7-12 minutes apart. I was assured that at some point they were closer together, but knowing they had plans to transport to the hospital to join her OB for a planned VBAC, I knew we first needed to get an established active labor pattern going. As a midwife I am only comfortable attending women in labor when I can listen to fetal heart tones in order to ensure fetal wellbeing. The baby sounded great and mom was handling her labor well. I suggested laboring in the bathtub with some Epsom salt in order to allow the contractions to regulate. She alternated positions from right side lying to left side lying every few contractions. Within minutes, contractions became more regular and were consistently 7.5 minutes apart. I monitored the baby’s heart rate regularly and we encouraged the mom to drink and take bites of fruit periodically. While the contractions never got closer than 6.5 minutes apart, I noticed the mom sounded “transition-y.” Difficult to describe or quantify, but in my experience there’s certain sounds a mom makes that tell you what point they are at in labor. I gently assured her and reminded her that, although we had just met this afternoon, I am a midwife and that I could perform a vaginal exam in order to let her know her progress. Remember, upon arrival just after 1pm, contractions had been irregular and now it was about 2pm, after only 1 hour in the bathtub. I shared my thoughts about her contraction pattern versus how she was physically presenting. After the next contraction we helped her out of the tub and to the bed for an exam. The next contraction she experienced was intense; this was the first one out of the tub and she voiced how much better she had been able to cope with them while in the water. With consent and sterile technique I gently performed an internal exam and found her almost complete with only an anterior lip (cervix in the front) and baby at +2 station. I calmly explained what I found and gave her time to process while we started the steps of getting her ready for transport. It was only 2:40pm. She was a trooper! I followed behind the client in my own vehicle, sterile gloves in my pocket just in case. We had discussed hospital arrival procedure and that I would park and run ahead to get a wheelchair so the mom could be dropped off at the front door and not have to walk much. I was blessed with a parking spot near the front entrance, which almost never happens, and ran ahead as planned to grab a wheelchair from the front. Empty. Nothing. And, to top it off, because it was Saturday, there were no workers or volunteers at the desk or anywhere to be found. Knowing this mom was ready to deliver at any moment, I couldn’t aimlessly walk around trying to locate someone who could help. Instead I went back out to help support the laboring mother. We labored through a couple contractions while her mother parked the car, and didn’t make much progress before she met up with us and the three of us walked inside. Still nothing or no one to help. The elevators were fairly close so we figured the best thing was to get there and up to Labor & Delivery. Once there, and it was a slow process, we finally found some help. We went from one to about five nurses and finally a wheelchair. We explained who she was, who her doctor was and what was going on. I was still supporting the mother and helped to ease her back into the wheelchair, which while it was welcome on one hand, was still difficult to do at this point. We quickly made it back to Labor and Delivery and they deduced based on her presentation that we could bypass triage and get a real room. I felt it prudent, because there were no less than seven nurses or staff buzzing about the room and the laboring mother, to let them know my assessment. Normally in this situation I would not advertise that I am a midwife, but I felt I really needed to let them know that I had done an exam and found her almost complete with baby +2. On top of the myriad of questions they were already asking her, this new revelation threw them and now they assumed, though we were already very clear about who this laboring mother was, who her doctor was, etc., that we were a transport from a home birth situation. No. That’s not what we said. Yes, I am a midwife. I am her labor support person who was helping her to labor at home until it was time to come to the hospital. She made quick progress and now we are here to meet her OB. More questions. Multiple times I tried to help and answer what I could for her; however, and this is the tricky part, the hospital staff wants to hear from the patient directly. Now, don’t get me wrong, I get this to some extent. We aren’t talking about possible abuse questions or suspicious injuries, we have a woman in advanced stages of labor, trying her best to birth a human being and we’re getting chatty. STOP IT! I digress. Now is the point where she is poked and prodded, because apparently those 36 week labs she just had aren’t considered relevant any longer and because the hospital has little to no regard for midwives, they can’t take my word about her internal exam, they need to see for themselves. Her second exam takes place at the hospital and is done by a nurse. She calls her 9 cm and says baby is +1 station. Then when asked by another nurse about this, she adds that there is only cervix in the front. (THAT’S CALLED AN ANTERIOR LIP!) But they don’t like to agree with the midwife. (And station, while subjective, could have changed given the car ride and anxiety the mother was in transporting at this stage of labor and her long walk to the delivery unit.) Her OB had not yet arrived because while she had called to let her know she had started labor that morning, they forgot to update her. That’s normal. When you are busy laboring, you aren’t thinking about everyone you should update. Instead, we had a hospitalist join the packed room in case the client/patient delivered prior to her OB’s arrival. At some point in this activity, I covered the mother with a light sheet because she wasn’t pushing yet, she was still laboring and I feel was waiting for her husband and then OB to arrive. Step in hospitalist/OB sub who moves the sheet and “needs” to check her again. WAIT, WHAT?!?! This is the part that continues to baffle me. Why do you allow nurses to do an internal exam if you aren’t going to believe their assessments? Either they are qualified or they are not. Why is this woman or any woman violated repeatedly with little to no regard for consent, all for the sake of routine practice? She had 3 internal exams by 3 different people in a matter of 40 minutes. That is completely unnecessary! Shortly after, the Doula I had been subbing for arrived and I graciously stepped aside to allow her to continue the role this laboring mother had hired her to perform. I was sad to miss out on the big moment, but I refused to add to the stress or crowd of the moment. By this point, the laboring mother had her husband, her mother, her original labor support person, and the hospital staff was no less than 4-6 people in the room because staff was still in and out. I didn’t want to be the point of contention and create an awkward moment where the soon-to-arrive OB states too many people are present and someone has to go. That would be rude of me; I had just met the couple that day. So, I politely excused myself and went to the waiting room because I knew the birth would be imminent. Roughly 15 minutes later I got the text that the baby had arrived and all was well. Sweet Bliss. Congratulations. This momma triumphed in so many ways. She did it, and she did more than she originally planned. I hope she looks back on the experience with lots of happiness, joy and maybe even some surprising funny moments that make her laugh out loud. But, I’m confused. This individual was under the care of an OB throughout her pregnancy. She did everything the system supports. Why, if this was the plan all along, was she questioned countless times by various staff, surrounded by more than a few people and forced to undergo multiple vaginal exams when she was basically complete? I just don’t get it. The hospitals ask the same questions routinely, do they not? Doctors ask the same questions, do they not? Is there a way for one system to talk to the other prenatally? People register at hospitals prior to delivery, right? Is there some sort of bracelet or barcode the expectant mom could wear (or bring in) that would answer those same questions allowing them to labor as uninterrupted as possible? Stop the madness. Labor is not the time to get super chatty with a woman who is literally working to bring a human being earth side. Please tell me you have ideas or you have the ear of someone who can help to change policy or systems. One hospital at a time, that’s all it takes! (It could start with a nurse or charge nurse or OB or hospital administrator…it only takes a spark to light a fire!) |
Melissa BatesExperience The Birth You've Always Imagined Archives
February 2020
Categories |
Location |
|
Copyright 2021 | My Radiant Beginnings LLC Website Designed With Love By The Creative Agency


 RSS Feed
RSS Feed
